Wednesday, February 29, 2012
Thursday, February 16, 2012
Monday, February 13, 2012
Hypercholesterolemia
Hypercholesterolemia:
Various clinical practice guidelines have addressed the treatment of hypercholesterolemia. The American College of Physicians has addressed hypercholesterolemia in patients with diabetes.[24] Their four recommendations are:
Various clinical practice guidelines have addressed the treatment of hypercholesterolemia. The American College of Physicians has addressed hypercholesterolemia in patients with diabetes.[24] Their four recommendations are:
- Lipid-lowering therapy should be used for secondary prevention of cardiovascular mortality and morbidity for all patients (both men and women) with known coronary artery disease and type 2 diabetes.
- Statins should be used for primary prevention against macrovascular complications in patients (both men and women) with type 2 diabetes and other cardiovascular risk factors.
- Once lipid-lowering therapy is initiated, patients with type 2 diabetes mellitus should be taking at least moderate doses of a statin (the accompanying evidence report states "simvastatin, 40 mg/d; pravastatin, 40 mg/d; lovastatin, 40 mg/d; atorvastatin, 20 mg/d; or an equivalent dose of another statin").[25]
lung Noules follow up
Fleischner Society Recommended Guidelines for follow-up and management of
nodules detected incidentally during non-screening CT examinations.
(MacMahon et al, Radiology 2005: 237; 395-400.)
NODULE SIZE (mm) - LOW-RISK PATIENT
? 4 No further follow up.
>4-6 CT at 12 months, if unchanged, no further follow-up.
>6-8 CT at 6-12 months then at 18-24 months if no change.
>8 CT at around 3, 9, and 24 months; or PET or biopsy.
NODULE SIZE (mm) - HIGH-RISK PATIENT
?4 CT at 12 mo, if unchanged, no further follow-up.
>4-6 CT at 6-12 mo then at 18-24 months if no change.
>6-8 CT at 3-6 mo then at 9-12 and 24 months if no change.
>8 CT at around 3, 9, and 24 months; or PET or biopsy.
nodules detected incidentally during non-screening CT examinations.
(MacMahon et al, Radiology 2005: 237; 395-400.)
NODULE SIZE (mm) - LOW-RISK PATIENT
? 4 No further follow up.
>4-6 CT at 12 months, if unchanged, no further follow-up.
>6-8 CT at 6-12 months then at 18-24 months if no change.
>8 CT at around 3, 9, and 24 months; or PET or biopsy.
NODULE SIZE (mm) - HIGH-RISK PATIENT
?4 CT at 12 mo, if unchanged, no further follow-up.
>4-6 CT at 6-12 mo then at 18-24 months if no change.
>6-8 CT at 3-6 mo then at 9-12 and 24 months if no change.
>8 CT at around 3, 9, and 24 months; or PET or biopsy.
Monday, January 30, 2012
Hypoxemic - Anoxic Brain injury
Several factors are important prognostic findings, particularly in patients who have not received significant sedation The outcome of hypoxic–ischaemic brain injury worsens if:
FOUR score (Full Outline of UnResponsiveness)
http://pn.bmj.com/content/11/1/4.full#F2
- The patient has been in coma (ie, unresponsive) for >6 h.
- There are no spontaneous limb movements or localisation to painful stimuli in the initial stages.
- There is prolonged loss of pupillary responses (provided atropine has not been administered).
- There is sustained conjugate eye deviation (upgaze or downgaze).
- There are specific forms of abnormal eye movements (eg, upbeat and downbeat nystagmus, ping pong gaze or period alternating nystagmus).
- There are myoclonic seizures.
- Lower cranial nerve function is involved (eg, absent cough and gag reflexes).
FOUR score (Full Outline of UnResponsiveness)
| Eye response | 4 | Eyelids open, tracking or blinking to command |
| 3 | Eyelids open but not tracking | |
| 2 | Eyelids closed but open to a loud voice | |
| 1 | Eyelids closed but open to pain | |
| 0 | Eyelids remain closed with pain | |
| Motor response | 4 | Thumbs-up, fist or peace sign |
| 3 | Localising to pain | |
| 2 | Flexion response to pain | |
| 1 | Extension response to pain | |
| 0 | No response to pain, or generalised myoclonic status | |
| Brainstem reflexes | 4 | Normal pupil and corneal reflexes present |
| 3 | One pupil wide and fixed | |
| 2 | Pupil or corneal reflexes absent | |
| 1 | Pupil and corneal reflexes absent | |
| 0 | Absent pupil, corneal and cough reflex | |
| Respiration | 4 | Not intubated, regular breathing pattern |
| 3 | Not intubated, Cheyne–Stokes breathing pattern | |
| 2 | Not intubated, irregular breathing pattern | |
| 1 | Breaths above ventilator rate | |
| 0 | Breaths at ventilator rate, or apnoea |
Interpretation of EKG
Interpretation of EKG's
Five Cardinal Features
- (1) Rate
- (2) Rhythm – including intervals
- (3) Axis
- (4) Hypertrophy
- (5) Infarction
- Three ways to determine rate:
- (1) count number of thick lines that occur between QRS complexes: 300 if next QRS on thick lines, 150 if 2nd, 100 if 3rd, then 75, 60, 50
- say: "300, 150, 100" "75, 60, 50" as counting thick lines
- can also use thin lines (thick lines bolded): 300, 250, 214, 187, 167; 150, 136, 125, 115, 107; 100, 94, 88, 83, 79; 75, 71, 68, 65, 62; 60
- (2) if bradycardic (less than 60 bpm) or irregular: count 6 second strip (2 3-second marks) and multiply by 10
- can also count entire strip (10 seconds) and multiply by 6
- (3) calculate: 1500/number of small lines between similar waves
- must determine coexisting independent rates if there are more than one
- Automaticity – heart has automaticity foci that respond at different rates and produce different morphology on EKG
- atrial – preceeded by P wave (shape of P wave changes depending upon originating focus), narrow complex QRS, normal rate 60-80/min
- junctional – no P wave, narrow QRS, normal rate 40-60/min
- ventricular – no P wave, wide QRS, normal rate 20-40/min
- Intervals
- PR should be less than 0.2 seconds (one large square)
- QRS should be less than 0.12 seconds (three small squares)
- QT interval – must be corrected for rate (QTc); in general, QT should be less than half R-R interval
- Sinus Rhythm – P before each QRS, QRS after each P, P in correct orientation (up in II)
- normal sinus rate is 60-100 bpm; if sinus rhythm but greater than 100 bpm, it is sinus tachycardia; if less than 60 bpm, it is sinus bradycardia
- Irregular Rhythms
- Sinus Arrythmia – varies with respiration, P waves identical; not pathological
- Wandering Pacemaker – irregular rhythm, P waves change shape, rate less than 100 bpm
- Multifocal Atrial Tachycardia – same as wandering pacemaker with rate greater than 100 bpm
- Atrial Fibrillation – irregular ventricular rhythm without P waves; may see erratic atrial spikes or wavy baseline
- Escape – lower level of heart will automatically respond if not driven with faster rate from above (automaticity)
- Escape Beat – single beat after a pause; can be atrial, junctional, or ventricular
- ventricular escape beats can be caused by burst of excessive parasympathetic activity (parasympathetic innervation inhibits SA node and AV junction but NOT ventricular tissue)
- Escape Rhythms – persistent escape beats (sinus node not active or not conducting); can be atrial, junctional ("idiojunctional" rhythm), or ventricular ("idioventricular" rhythm)
- idiojunctional rhythms can produce retrograde atrial depolarization with an inverted P' before, during, or after the QRS
- idioventricular rhythms caused by complete block below AV junction (P waves present but not associated with QRS) or total failure of all tissue above ventricles (downward displacement of the pacemaker)
- idioventricular rhythms can cause loss of consciousness due to insufficient cardiac output (Stokes-Adams Syndrome)
- Premature Beats – from an irritable automaticity focus; can be atrial (PAB), junctional (PJB), or ventricular (PVC; 6 PVC's per minute is pathological)
- PAB/PJB – irritable atrial and junctional foci are caused by sympathetic stimulation, caffeine, amphetamines, cocaine, digitalis, toxins, ethanol, hyperthyroidism, and stretch receptors
- PAB resets from the new P' wave at previous rate (first cycle slightly lengthened due to transient baroreceptor reflex)
- PAB's can cause wide QRS (aberrent ventricular conduction)
- PAB and PJB still depolarize the SA node (either directly or through retrograde atrial depolarization) and reset the pacing, so rhythm begins again in phase with the premature beat
- if the beat is not conducted (due to refractoriness), the missed QRS in produces a long empty baseline (harmless)
- can occur every other beat (atrial or junctional bigeminy) or every third beat (atrial or junctional trigeminy)
- PVC – irritable ventricular foci are caused by low oxygen, hypokalemia, or muscle pathology (mitral valve prolapse, myocarditis, etc.)
- PVC's do not depolarize the SA node, so there is a "compensatory" pause after them (except for "interpolated" PVC's, where they occur exactly where the ventricular contraction would have)
- P waves continue unaffected and the next QRS occurs where it would have if there had been no PVC
- a PVC that falls on a T wave ("R on T phenomenon") can cause sustained ventricular tachycardia
- ventricular parasystole – ventricular tissue with entrance block (NOT an irritable focus) that starts PVC's at its own automatic firing rate
- Tachyarrhythmias
- Paroxysmal tachycardia – 150-250 bpm; can be atrial (PAT), junctional (PJT), or ventricular (PVT)
- atrial (PAT) or junctional (PJT) are also called paroxysmal superventricular tachycardia (PSVT)
- paroxysmal atrial tachycardia with block (PAT with more than one P wave before each QRS) – caused by digitalis
- AV nodal reentry tachycardia (AVNRT) is a type of PJT
- PJT may still have retrograde atrial depolarization and inverted P' waves
- PJT may involve somewhat widened QRS since one bundle branch may still be refractory when next beat arrives (aberrent ventricular conduction)
- PVT:
- during PVT, if the P wave appears at just the right time, can see normal QRS (capture beat) or QRS that degenerates into a PVC (fusion beat)
- PVT can be distinguished from PSVT with wide QRS (caused by BBB, etc.) by the following:
- presence of coronary artery disease
- very wide QRS (more than 0.14 sec)
- extreme RAD
- AV dissociation (see capture or fusion beats)
- Torsades des Pointes – "party streamer"; caused by two competitive, irritable foci in different ventricular areas
- Flutter – 250-350 bpm; can be atrial (sawtooth baseline with QRS's) or ventricular (sine wave; almost always leads to fibrillation unless treated)
- Fibrillation – greater than 350 bpm; can be atrial (jagged baseline with QRS's) or ventricular (no identifiable waves)
- no pumping occurs
- atrial fibrillation can produce a narrow-complex tachycardia (rapid ventricular response)
- Block – identify by pauses (sinus block), abnormal PR intervals (AV blocks), abnormal QRS interval (bundle branch block), or axis deviation (hemiblock)
- Sinus Block – spontaneous pause in electrical activity; can restart automatically or have an escape beat (see above)
- AV Block – causes abnormal PR interval
- 1st degree block – PR too long (greater than 0.2 seconds, or one large square)
- 2nd degree block – some P waves without QRS:
- Wenkebach (Mobitz I) – block at the node itself; PR gradually lengthens until a P does not produce a QRS
- Mobitz II – block beyond the node; PR length constant, but some P waves do not produce QRS (can be 2:1, 3:1, etc., or even intermittent)
- 2:1 block can be either of above; can use vagal maneuvers to differentiate (see below)
- 3rd degree block – none of the P waves get through; there is an idioventricular or idiojunctional rate instead
- Bundle Brach Block – basically two out of phase QRS's (R R'); requires wide QRS for diagnosis (at least 3 small squares; best to use limb leads since low voltages allow for more accurate measurement)
- Right Bundle Branch Block (RBBB) – QRS has two peaks (R R') in V1 or V2 usually returning to lower than baseline between them
- Left Bundle Branch Block (LBBB) – QRS has two peaks (R R') in V5 or V6 with slight depression between them
- BBB makes ventricular hypertrophy criteria unreliable
- LBBB makes infarction difficult to determine
- BBB can cause SVT to degenerate more easily into VT
- Hemiblock – block of anterior or posterior fascicle of LBB; causes axis deviation and widened QRS
- Anterior hemiblock – left axis deviation with a Q wave in I and a prominent S wave in III
- Posterior hemiblock – right axis deviation with a prominent S wave in I and a Q wave in III
- can have bifascicular blocks (RBBB + hemiblock)
- must have previous EKG to diagnose so that other causes of axis deviation can be ruled out
- Vagal Maneuvers (gagging or carotid sinus massage) – inhibit irritable atrial or junctional foci or increase the refractoriness of the AV node
- abolishes PSVT, identifies 2:1 AV block (no effect if Mobitz II), and reveals flutter waves in atrial flutter
- find axis quadrant using below diagram (QRS above or below baseline in each lead):
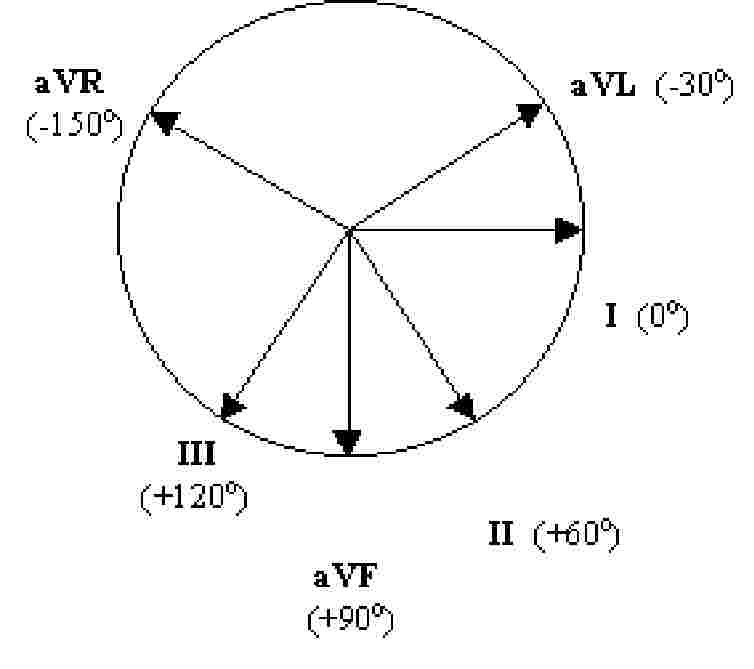
- axis is also 90 degrees from isoelectric QRS (same up as down) or in the direction of a QRS that only goes up (opposite direction of QRS that only goes down)
- Normal axis is "up in I and aVF" (some say "up in I and II")
- if I is down: right axis deviation (RAD)
- if aVF is down: left axis deviation (LAD)
- if both are down: extreme RAD
- Axis Rotation – find isoelectric QRS (same up as down) in chest leads (V1 to V6); normally occurs in V3 or V4
- if isoelectric in V1 or V2: rightward rotation
- if isoelectric in V5 or V6: leftward rotation
- Atrial Hypertrophy – diphasic P wave in V1
- right atrial hypertrophy – large initial component of diphasic P wave in V1
- left atrial hypertrophy – large terminal component of diphasic P wave in V1
- Ventricular Hypertrophy – tall R wave in V1 for RVH, deep S wave in V1 and tall R wave in V5 for LVH
- right ventricular hypertrophy – widened QRS with RAD, rightward rotation, and:
- R greater than S in V1 but R gets smaller in V2 through V6
- S wave persists in V5 and V6
- left ventricular hypertrophy – widened QRS with LAD, leftward rotation, and:
- sum of depth of S in V1 and height of R in V5 is more than 35 small squares
- inverted T wave with gradual downslope and rapid upslope
Infarction – always requires previous EKG for comparison
- Identifying Injury
- (1) ischemia – inverted T waves (earliest sign) – symmetrical down- and upslope, opposite direction of QRS
- (2) acute injury – ST elevation
- can occur without Q waves: "non Q-wave MI"
- ST depression may indicate "subendocardial infarction" (small shallow area as opposed to entire wall of heart)
- (3) necrosis (non-conductive tissue) – Q-waves
- significant if more than one small square wide or greater than 1/3 the amplitude of the QRS
- remain even after acute infarction is over (unlike other two)
- Localizing Injury – leads where the above occur; also remember that axis points away from infarction
- Anterior – left anterior descending artery – V1 to V4
- Lateral – circumflex artery – I, aVL
- Inferior – right or left coronary artery – II, III, aVF
- Posterior – right coronary artery – V1 and V2, but changes are mirror image (R instead of Q, ST depression instead of elevation, etc.)
- for blocks and hemiblocks: AV node is supplied by the right coronary artery, RBB and anterior LBB is supplied by LAD, posterior LBB is supplied by either
- Pulmonary Embolism
- prominent S wave in I
- Q wave in III
- inverted T waves in III and V1 through V4
- ST depression in II
- acute incomplete RBBB
- RAD with rightward rotation
- Electrolyte Disturbances
- hyperkalemia
- wide flat P – P disappears entirely with severe hyperkalemia
- wide QRS
- peaked T wave
- hypokalemia
- flat T wave
- U wave (after T wave; represents Purkinje cell repolarization) – prominent with severe hypokalemia
- can cause torsades des pointes if extreme
- hypercalcemia – shortened QT interval
- hypocalcemia – prolonged QT interval
- Drugs
- Digitalis
- therapeutic – ST slopes below baseline, inverted T waves, shortened QT
- excessive – blocks: SA block, paroxysmal atrial tachycardia (PAT) with block, AV block (can be 3rd degree)
- toxic – atrial fibrillation, junctional or ventricular tachycardia, frequent PVC's, ventricular fibrillation
- Quinidine (blocks potassium channels)
- wide notched P wave
- wide QRS
- very deep ST
- U wave
- long QT interval
- Pericarditis
- flat or concave downward ST segment elevation in leads where QRS is mainly negative (right chest leads – V1 to V3)
- elevated ST segment with T wave off baseline in leads where QRS is mainly positive (lateral/inferior limb leads – aVL, I, II, aVF, III)
- COPD
- all waves of minimal amplitude; often leads to RVH with RAD; MAT in some cases
- Wolff-Parkinson-White Syndrome – caused by accessory bundle of Kent that bypasses the AV node to allow ventricular pre-excitation
- delta wave with apparently shortened PR interval
- can cause tachycardia through three mechanisms:
- (1) rapid conduction of rapid atrial beats (PSVT, atrial flutter, or atrial fibrillation)
- (2) automaticity foci within the bundle
- (3) re-entry of ventricular depolarization
- Lown-Ganong-Levine Syndrome – caused by James bundle (extention of the anterior internodal tract) that bypasses the AV node directly to the bundle of His
- no PR delay (so PR interval is minimal)
- QRS immediately responds to any atrial tachyarrythmias, so (for example) atrial flutter produces a rapid QRS response
- Brugada Syndrome – familial dysfunction of Na+ channels
- characterized by RBBB with ST elevation (downsloping) in V1 through V3
- can cause deadly arrythmias leading to sudden cardiac death with no apparent structural heart disease (responsible for half of all cases)
- Wellen's Syndrome – stenosis of LAD
- causes marked T-wave inversion in V2 and V3
- Long QT Syndrome – QT interval more than 1/2 the cardiac cycle
- predisposed to ventricular arrythmias
Hypertensive Urgency vs Emergrncy
-Urgency: is increase in BP > 180 / 120 w/o any signs of target organ damage
-while emergency: is increase in BP > 180/120 w s/o target organ damage , like:
-while emergency: is increase in BP > 180/120 w s/o target organ damage , like:
- Flash pulm edema- do CXR
- CVA: get CTB
- renal failure: get BUN and Cr
- Coronary ischemia/ infarction: get EKG and Cardiac Enzymes
Management:
for Urgency:: goal is to decrease BP by 25% in next 24 hrs
While for Emergency : goal is to decrease BP by 10% in next 1 hr and 25 in next 3- 4 hrs
Pathophysiology:
High BP--cause damage to endothelium---> Decrease NO secretion---> further exacerbates BP
Also Due to Endothelin damage ---> there will be Capillary leakage --> causing Flash Pulm Edema
Wednesday, January 25, 2012
Monday, January 23, 2012
Hypoxemia
If pt is getting Hypoxemia---> give High FiO2---> improving then
does not improve---> increase PEEP:
does not improve---> increase PEEP:
Pressors
- Septic Shock: use Either Dopa or Levophed---> if u started with either of them then next of choice is Vasopressin--> if still low then add the one that u did not use before ( from Dopa or Levophed)
- Anaphylactic Shock: Epinephrine
- BP is low but stable, Heart failure and Pt is getting Acute pulmonary Edema / or other organ failure 2/2 Cardiogenic SHock then use Dobutamine
Tuesday, January 10, 2012
brainstem syndrome
Claude's syndrome is caused by midbrain infarction as a result of occlusion of a branch of the posterior cerebral artery. This lesion is usually a unilateral infarction of the red nucleus and cerebral peduncle, affecting several structures in the midbrain including:
| Structure damaged | Effect |
|---|---|
| dentatorubral fibers | contralateral ataxia |
| corticospinal tractfibers | contralateral hemiparesis |
| corticobulbar tractfibers | contralateral hemiplegia of lower facial muscles, tongue, and shoulder |
| oculomotor nerve fibers | ipsilateral oculomotor nerve palsy with a drooping eyelid and fixed wide pupil pointed down and out; probablediplopia |
Bnedikt:
It is characterized by the presence of an CN III oculomotor nerve palsy and cerebellar ataxia including tremor. Neuroanatomical structures affected include CNIII nucleus, Red nucleus, corticospinal tracts, brachium conjunctivum, and cerebellum. It is very similar in etiology, morphology and clinical presentation to Weber's syndrome; the main difference between the two being that Weber's is more associated with hemiplegia (i.e. paralysis), and Benedikt's with hemiparesis (i.e. weakness).
Foville's syndrome is caused by the blockage of the perforating branches of the basilar artery in the region of the brainstem known as thepons.[1]
Structures affected by the infarct are the PPRF, nuclei of cranial nerves VI and VII, corticospinal tract, medial lemniscus, and the medial longitudinal fasciculus.
Millard-Gubler syndrome
Symptoms result from the functional loss of several anatomical structures of the pons, including the sixth and seventh cranial nerves and fibers of the corticospinal tract. Paralysis of the abducens (CN VI) leads to diplopia, internal strabismus, and loss of power to rotate the affected eye outward), and disruption of the facial nerves (CN VII) leads to symptoms including flaccid paralysis of the muscles of facial expression and loss of the corneal reflex. Disruption of the corticospinal tract leads to contralateral hemiplegia of the extremities.
It is a form of "crossed hemiplegia," as the paralysis of muscles controlled by the facial nerve occurs on the same side as the lesion, while the hemiplagia of muscles below the neck occurs on the opposite side as the lesion.

